Keywords
Abstract
Introduction: Submental intubation provides a valuable alternative in maxillofacial fracture surgery when oral and nasal routes are contraindicated. A key advantage is that it allows for dental occlusion, which is necessary for proper alignment of fractured bone fragments. Despite its benefits, this technique remains underutilised in Malaysia due to limited research, training, and exposure among anaesthesiologists. Therefore, this study explores the types of maxillofacial fractures as well as the indications and complications of submental intubation.
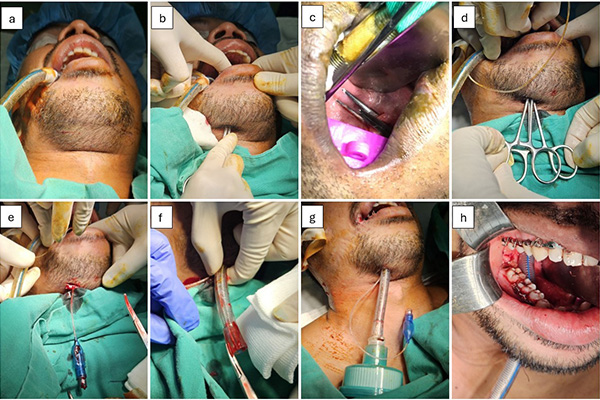
Methods: This was a retrospective study using the census sampling technique. A total of 11 patients who underwent submental intubation via a paramedian approach with double haemostats at Hospital Teluk Intan between January 2022 and March 2025 were reviewed. Immunocompromised patients were excluded. A descriptive analysis was performed on the types of maxillofacial fractures, indications for submental intubation and postoperative complications.
Results: Data from 11 patients were analysed. Seven patients (63.6%) sustained combined midface and mandibular fractures, 3 patients (27.3%) had midface fractures, and 1 patient (9.1%) had mandibular fracture. Additionally, 7 patients (63.6%) presented with nasal bone and/or septum fractures, 2 patients (18.2%) had skull base fracture, and 2 patients (18.2%) had combined fractures of nasal bone, septum, and skull base. One patient developed a postoperative infection and hypertrophic scar, while the remaining 10 recovered uneventfully. The observed complication rate was 9.1% (95% CI: 0.2%–40.3%).
Conclusion: Submental intubation appears to be a safe and feasible alternative with minimal complications. Larger studies are needed to validate these preliminary findings.
References
Lim D, Ma BC, Parumo R, Shanmuhasuntharam P. Thirty years of submental intubation: a review. Int J Oral Maxillofac Surg. 2018;47:1161-1165. http://doi.org/10.1016/j.ijom.2018.04.015
Park KN, Karm MH. Submental/submandibular intubation: a journey from past to future. Anesth Pain Med. 2024;19(4):280-293. http://doi.org/10.17085/apm.24120
De Toledo GL, Bueno SC, Mesquita RA, et al. Complications from submental endotracheal intubation: a prospective study and literature review. Dent Traumatol. 2013;29:197-202. http://doi.org/10.1111/edt.12032
Williams KA, Tariq M, Acharekar MV, et al. Submental intubation in maxillofacial procedures: a more desired approach than nasotracheal intubation and tracheostomy. Cureus. 2022;14(7):e27475. http://doi.org/10.7759/cureus.27475
Das S, Das TP, Ghosh PS. Submental intubation: a journey over the last 25 years. J Anaesthesiol Clin Pharmacol. 2012;28(3):291-303. http://doi.org/10.4103/0970-9185.98320
Jundt JS, Cattano D, Hagberg CA, et al. Submental intubation: a literature review. Int J Oral Maxillofac Surg. 2012;41:46-54. http://doi.org/10.1016/j.ijom.2011.08.002
Goh EZ, Loh NHW, Loh JSP. Submental intubation in oral and maxillofacial surgery: a systematic review 1986–2018. Br J Oral Maxillofac Surg. 2020;58(1):43-50. http://doi.org/10.1016/j.bjoms.2019.10.314
Scafati CT, Maio G, Aliberti F, et al. Submento-submandibular intubation: is the subperiosteal passage essential? Experience in 107 consecutive cases. Br J Oral Maxillofac Surg. 2006;44:12-14. http://doi.org/10.1016/j.bjoms.2005.07.011
Tidke AS, Borle RM, Madan RS, et al. Transmylohyoid/submental endotracheal intubation in panfacial trauma: a paradigm shift in airway management with prospective study of 35 cases. Indian J Otolaryngol Head Neck Surg. 2013;65:255-259. http://doi.org/10.1007/s12070-012-0505-x
McGinty S, Siddiqui WJ. Keloid. Treasure Island (FL): StatPearls Publishing [Internet]; [cited 2025 Jan 1]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507899/