Keywords
Abstract
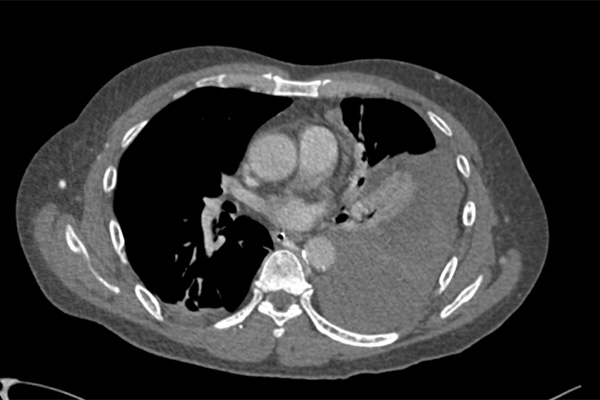
Massive haemothorax is a rare but life-threatening complication of internal jugular vein catheterisation. We report a 55-year-old male with end-stage renal failure and limited intravascular access who required a tunnelled dialysis catheter after fistula failure and missed haemodialysis. Multiple ultrasound-guided insertion attempts resulted in an inadvertent massive left haemothorax. The patient developed immediate postprocedural respiratory distress, requiring intensive care unit (ICU) admission, mechanical ventilation, and vasopressor support. Computed tomography of the thorax confirmed left sided haemothorax, and an ultrasound-guided chest tube was inserted. It drained 700 mL of blood. He received transfusion of 4 units each of packed red blood cells, fresh frozen plasma, cryoprecipitate, and platelets. After stabilisation, he was transferred urgently to a tertiary hospital for cardiothoracic surgery. Thoracotomy revealed subclavian vein injury, which was repaired with an estimated intraoperative blood loss of 1.8 L. Postoperatively, he was successfully weaned from mechanical ventilation over 4 days in ICU. Early recognition of this rare complication and timely definitive intervention is essential to improving outcomes and ensuring patient safety.
References
Infant J, Russell I, Snell J, et al. Applied Anatomy for the FRCA. 2nd ed. Cambridge: Cambridge University Press; 2012.
Maya ID, Allon M. Vascular access: core curriculum 2008. Am J Kidney Dis. 2008;51(4):702-8. http://doi.org/10.1053/j.ajkd.2007.10.046
Lamperti M, Bodenham AR, Pittiruti M, et al. International evidence-based recommendations on ultrasound-guided vascular access. Intensive Care Med. 2012;38(7):1105-17. http://doi.org/10.1007/s00134-012-2597-x
Pumarejo Gomez L, Tran VH. Hemothorax. 2023 Aug 8 [updated 2025 Jan]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538219/
Zeiler J, Idell S, Norwood S, Cook A. Hemothorax: a review of the literature. Clin Pulm Med. 2020;27(1):1-12. http://doi.org/10.1097/CPM.0000000000000343
Taylor LA, Stenberg R, Tozer J, Vitto MJ, Joyce M, Jennings J, et al. Novel approach to ultrasound-guided thoracostomy. J Ultrasound Med. 2022;41(3):743-7. http://doi.org/10.1002/jum.15759
Inaba K, Lustenberger T, Recinos G, Georgiou C, Velmahos GC, Brown C, et al. Does size matter? A prospective analysis of 28–32 versus 36–40 French chest tube size in trauma. J Trauma Acute Care Surg. 2012;72(2):422-7. http://doi.org/10.1097/TA.0b013e3182452444
Bauman ZM, Kulvatunyou N, Joseph B, et al. Randomized clinical trial of 14-French (14F) pigtail catheters versus 28–32F chest tubes in the management of patients with traumatic hemothorax and hemopneumothorax. World J Surg. 2021;45(3):880-6. http://doi.org/10.1007/s00268-020-05852-0
Tanizaki S, Maeda S, Sera M, et al. Small tube thoracostomy (20–22 Fr) in emergent management of chest trauma. Injury. 2017;48(9):1884-7. http://doi.org/10.1016/j.injury.2017.06.021
UpToDate [Internet]. Waltham (MA): UpToDate; 2025 [cited 2025 Mar 4]. Available from: https://www.uptodate.com/contents/initial-evaluation-and-management-of-blunt-thoracic-trauma-in-adults?search=massive%20hemothorax&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
American Society of Anesthesiologists Task Force on Central Venous Access. Practice guidelines for central venous access 2020: an updated report. Anesthesiology. 2020;132(1):8-43. http://doi.org/10.1097/ALN.0000000000002864
Singh R, Yadav G, Goudra B. Difficult internal jugular central venous cannulation using ultrasound guidance. Case Rep Anesthesiol. 2019;2019:5134575. http://doi.org/10.1155/2019/5134575
Katiyar S, Jain RK, Bihari V. Entrapped central venous catheter guide wire. J Anaesthesiol Clin Pharmacol. 2010;26(3):406-7. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC2943714/
Chui J, Saeed R, Jakobson DJ, et al. Is routine chest radiography necessary after ultrasound-guided central venous catheter insertion? Chest. 2018;154(1):120-6. http://doi.org/10.1016/j.chest.2018.03.020
Sharma A, Bodenham A. Futility of “routine” postprocedural chest radiograph after hemodialysis catheter insertion. J Vasc Access. 2018;19(3):207-9. http://doi.org/10.1177/1129729817747622
Zehtabchi S, Sinert R, Goldman M, Kapitanyan R, Ballas J. Diagnostic performance of serial hematocrit measurements in identifying major injury in adult trauma patients. Injury. 2006;37(1):46-52. http://doi.org/10.1016/j.injury.2005.05.033
Lasek J, Jadczuk E. Thoracic trauma – principles of surgical management. Eur J Transl Clin Med. 2020;3(2):47-55. http://doi.org/10.31373/ejtcm/120124