Keywords
Abstract
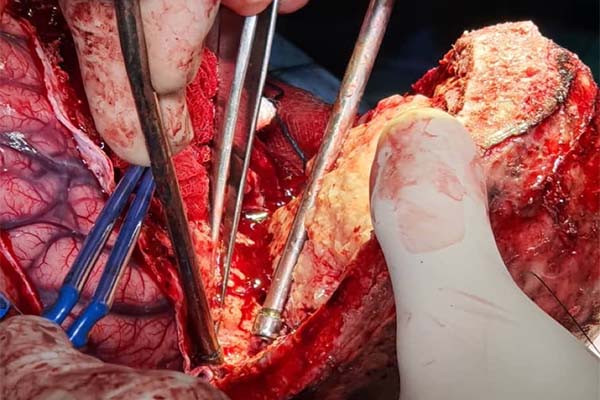
In Wolff-Parkinson-White (WPW) syndrome, the presence of an accessory pathway between the atrium and ventricle predisposes the patient to paroxysmal supraventricular tachyarrhythmias, which may progress to ventricular fibrillation and sudden cardiac death. Several drugs that are used perioperatively may alter the cardiac conduction velocity and refractory period. This fact, interacting with factors such as increased sympathetic tone (e.g., anxiety, pain, or seizure) or haemorrhage, leads to tachycardia, where shortened R-R interval predisposes the heart to re-entrant tachyarrhythmias. We reported and highlighted the perioperative issues while anaesthetising a 15-year-old boy with WPW syndrome for craniotomy and excision of parietal meningioma.
References
Pediatric and Congenital Electrophysiology Society (PACES), Heart Rhythm Society (HRS), American College of Cardiology Foundation (ACCF), American Heart Association (AHA), American Academy of Pediatrics (AAP), Canadian Heart Rhythm Society (CHRS). PACES/HRS expert consensus statement on the management of the asymptomatic young patient with a Wolff-Parkinson-White (WPW, ventricular preexcitation) electrocardiographic pattern: developed in partnership between the PACES and the HRS. Endorsed by the governing bodies of PACES, HRS, the ACCF, the AHA, the AAP, and the CHRS. Heart Rhythm. 2012;9(6):1006-24. https://doi.org/10.1016/j.hrthm.2012.03.050
Bengali R, Wellens HJJ, Jiang Y. Perioperative management of the Wolff-Parkinson-White Syndrome. J Cardiothorac Vasc Anesth. 2014;28(5):1375-86. https://doi.org/10.1053/j.jvca.2014.02.003
De Bacquer D, De Backer G, Kornitzer M. Prevalences of ECG findings in large population-based samples of men and women. Heart. 2000;84:625-33. https://doi.org/10.1136/heart.84.6.625
Vladinov G. Fermin L, Longini R, et al. Choosing the anesthetic and sedative drugs for supraventricular tachycardia ablations: a focused review. Pacing Clin Electrophysiol. 2018;41(11):1555-63. https://doi.org/10.1111/pace.13511
Shwayder MH, Escudero CA, Etheridge SP, et al. Difficulties with invasive risk stratification performed under anesthesia in pediatric Wolff-Parkinson-White Syndrome. Heart Rhythm. 2020 Feb;17(2):282-6. https://doi.org/10.1016/j.hrthm.2019.09.011
Etheridge SP, Escudero CA, Blaufox AD, et al. Life-threatening event risk in children with Wolff-Parkinson-White Syndrome. JACC Clin Electrophysiol. 2018 Apr;4(4):433-44. https://doi.org/10.1016/j.jacep.2017.10.009
Fujii K, Iranami H, Nakamura Y, Hatano Y. High-dose remifentanil suppresses sinoatrial conduction and sinus node automaticity in pediatric patients under propofol-based anesthesia. Anesth Analg. 2011 May;112(5):1169-73. https://doi.org/10.1213/ANE.0b013e318210f4ef
Seki S, Ichimiya T, Tsuchida H, Namiki A. A case of normalisation of Wolff-Parkinson-White Syndrome conduction during propofol anesthesia. Anesthesiology. 1999 June;90(6):1779-81. https://doi.org/10.1097/00000542-199906000-00038
Sengul T, Saracoglu A, Sener S, Bezen O. Case report: the use of sugammadex in a pregnant patient with Wolff-Parkinson-White syndrome. J. Clin. Anesth. 2016; 33:1-4. https://doi.org/10.1016/j.jclinane.2015.12.023
Yang J, Cheng H, Shang R, et al. Hemodynamic changes due to infiltration of the scalp with epinephrine-containing lidocaine solution: a hypotensive episode before craniotomy. J Neurosurg Anesthesiol. 2007 Jan;19(1):31-7. https://doi.org/10.1097/01.ana.0000211023.34173.5e
Koch KU, Mikkelsen IK, Aanerud J, et al. Ephedrine versus phenylephrine effect on cerebral blood flow and oxygen consumption in anesthetized brain tumor patients: a randomized clinical trial. Anesthesiology. 2020 Aug;133(2): 304-17. https://doi.org/10.1097/ALN.0000000000003377