Keywords
Abstract
Introduction: Sepsis is the leading cause of intensive care unit (ICU) admission. Delayed recognition of sepsis is associated with increased morbidity and mortality. Monocyte distribution width (MDW) represents the width of a set of monocyte volume values, which increases as infections progress in severity. This study evaluated the diagnostic and prognostic accuracy of MDW and white cell count (WCC) for sepsis and mortality.
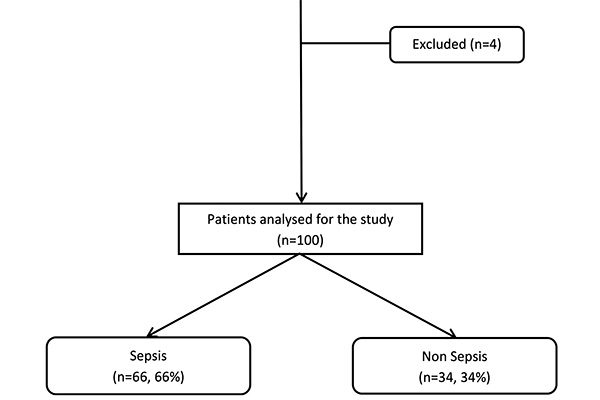
Methods: This was a prospective cohort study of 100 patients who were grouped into sepsis and non-sepsis according to the Sepsis-3 definition. MDW and WCC were collected on admission to ICU and for the subsequent 3 days.
Results: On admission, MDW was diagnostic of sepsis with an AUC of 0.86 (95% CI, 0.7–0.94) with a cut-off threshold of 20.97. Serial MDW on days 1 and 2 were also shown to be predictive of sepsis. MDW has a high sensitivity of 92.1% (95% CI, 82.4–97.4%) but a specificity of only 68.8% (95% CI, 50.0– 83.9%). The positive predictive value and negative predictive value of MDW using the new cut-off threshold in this study were found to be 83.6% (95% CI, 73–91.2 %) and 81.5% (95% CI, 61.9–93.7%), respectively.
Conclusions: MDW is an effective screening tool in the detection of sepsis upon admission to the ICU. As part of the differential in some complete blood count analysis machines, MDW provides a cost-effective and widely available test at present. Early detection of sepsis allows initiation of sepsis care bundle and better clinical outcomes.
References
Li T, Tan LD, Cheng C. Malaysian Registry of Intensive Care Report for 2015 Technical Committee of the Malaysian Registry of Intensive Care. Available from: www.mric.org.my
Seymour CW, Kahn JM, Martin-Gill C, et al. Delays From First Medical Contact to Antibiotic Administration for Sepsis. Crit Care Med. 2017 May;45(5):759-765. https://doi.org/10.1097/CCM.0000000000002264
Jones SL, Ashton CM, Kiehne L, et al. Reductions in Sepsis Mortality and Costs After Design and Implementation of a Nurse-Based Early Recognition and Response Program. Jt Comm J Qual Patient Saf. 2015 Nov;41(11):483-91. https://doi.org/10.1016/s1553-7250(15)41063-3
Pruinelli L, Westra BL, Yadav P, et al. Delay Within the 3-Hour Surviving Sepsis Campaign Guideline on Mortality for Patients With Severe Sepsis and Septic Shock. Crit Care Med. 2018 Apr;46(4):500-505. https://doi.org/10.1097/CCM.0000000000002949
Liu VX, Fielding-Singh V, Greene JD, et al. The Timing of Early Antibiotics and Hospital Mortality in Sepsis. Am J Resp Crit Care Med. 2017;196(7):856-863. https://doi.org/0.1164/rccm.201609-1848OC
Crouser ED, Parrillo JE, Seymour C, et al. Improved Early Detection of Sepsis in the ED With a Novel Monocyte Distribution Width Biomarker. Chest. 2017 Sep;152(3):518-526. https://doi.org/10.1016/j.chest.2017.05.039
Ljungström L, Pernestig AK, Jacobsson G, Andersson R, Usener B, Tilevik D. Diagnostic accuracy of procalcitonin, neutrophil-lymphocyte count ratio, C-reactive protein, and lactate in patients with suspected bacterial sepsis. PLoS One. 2017 Jul 20;12(7):e0181704. https://doi.org/10.1371/journal.pone.0181704
Kim MJ, Cheng G, Agrawal DK. Cl-channels are expressed in human normal monocytes: a functional role in migration, adhesion and volume change. Clin Exp Immunol. 2004;138(3):453-459. https://doi.org/10.1111/j.1365-2249.2004.02635.x
Leckie MJ. Automated quantitation of circulating neutrophil and eosinophil activation in asthmatic patients. Thorax. 2000;55(6):471-477. https://doi.org/10.1136/thorax.55.6.471
Mifsud EJ, Tan ACL, Jackson DC. TLR Agonists as Modulators of the Innate Immune Response and Their Potential as Agents Against Infectious Disease. Front Immunol. 2014;5(MAR). https://doi.org/10.3389/fimmu.2014.00079
Mukherjee R, Kanti Barman P, Kumar Thatoi P, Tripathy R, Kumar Das B, Ravindran B. Non-Classical monocytes display inflammatory features: Validation in Sepsis and Systemic Lupus Erythematous. Sci Rep. 2015 Sep 11;5:13886. https://doi.org/10.1038/srep13886
Goasguen JE, Bennett JM, Bain BJ, Vallespi T, Brunning R, Mufti GJ. Morphological evaluation of monocytes and their precursors. Haematologica. 2009;94(7):994-997. https://doi.org/10.3324/haematol.2008.005421
Crouser ED, Parrillo JE, Seymour CW, et al. Monocyte Distribution Width: A Novel Indicator of Sepsis-2 and Sepsis-3 in High-Risk Emergency Department Patients. Crit Care Med. 2019 Aug;47(8):1018-1025. https://doi.org/10.1097/CCM.0000000000003799
Piva E, Zuin J, Pelloso M, Tosato F, Fogar P, Plebani M. Monocyte distribution width (MDW) parameter as a sepsis indicator in intensive care units. Clin Chem Lab Med. 2021 Mar 5;59(7):1307-1314. https://doi.org/10.1515/cclm-2021-0192
Agnello L, Sasso B, Giglio RV, et al. Monocyte distribution width as a biomarker of sepsis in the intensive care unit: A pilot study. Ann Clin Biochem. 2021;58(1):70-72. https://doi.org/10.1177/0004563220970447
Obuchowski NA. Sample size calculations in studies of test accuracy. Stat Methods Med Res. 1998;7(4):371-392. https://doi.org/10.1191/096228098678080061
Woo A, Oh DK, Park CJ, Hong SB. Monocyte distribution width compared with C-reactive protein and procalcitonin for early sepsis detection in the emergency department. PloS One. 2021;16(4):e0250101. https://doi.org/10.1371/journal.pone.0250101
Hausfater P, Robert Boter N, Morales Indiano C, et al. Monocyte distribution width (MDW) performance as an early sepsis indicator in the emergency department: comparison with CRP and procalcitonin in a multicenter international European prospective study. Crit Care. 2021 Jun 30;25(1):227. https://doi.org/10.1186/s13054-021-03622-5
Agnello L, Bivona G, Vidali M, et al. Monocyte distribution width (MDW) as a screening tool for sepsis in the Emergency Department. Clin Chem Lab Med. 2020;58(11):1951-1957. https://doi.org/10.1515/cclm-2020-0417
Agnello L, Bivona G, Vidali M, et al. Monocyte distribution width (MDW) as a screening tool for sepsis in the Emergency Department. Clin Chem Lab Med. 2020 Oct 25;58(11):1951-1957. https://doi.org/10.1515/cclm-2020-0417
Mat-Nor MB, Md Ralib A, Abdulah NZ, Pickering JW. The diagnostic ability of procalcitonin and interleukin-6 to differentiate infectious from noninfectious systemic inflammatory response syndrome and to predict mortality. J Crit Care. 2016 Jun;33:245-51. https://doi.org/10.1016/j.jcrc.2016.01.002
Md Ralib A, Mat Nor MB, Pickering JW. Plasma Neutrophil Gelatinase-Associated Lipocalin diagnosed acute kidney injury in patients with systemic inflammatory disease and sepsis. Nephrology (Carlton). 2017 May;22(5):412-419. https://doi.org/10.1111/nep.12796
Agnello L, lo Sasso B, Bivona G, et al. Reference interval of monocyte distribution width (MDW) in healthy blood donors. Clinica Chimica Acta. 2020;510:272-277. https://doi.org/10.1016/j.cca.2020.07.036