Keywords
Abstract
Introduction: The use of audiovisual feedback devices on chest compression (CC) metrics such as the rate and depth has been proven to improve resuscitation quality. This study compared the quality of CC performed by anaesthetic trainees on manikins with audiovisual feedback and subsequent skill retention without the feedback.
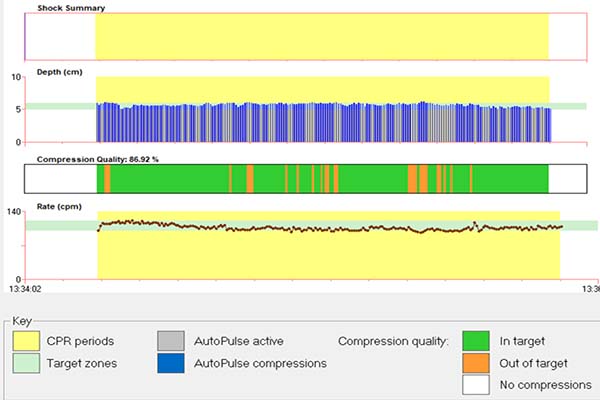
Methods: CC metrics measured were the compression rate and depth recorded and reviewed by RescueNet® Code Review software, which recorded compressions in target. Fifty participants performed 2 minutes of CC without audiovisual feedback (CC1), followed by another 2 minutes of CC with audiovisual feedback (CC2), separated by 5 minutes of rest. Those who achieved at least 70% of compressions in target during CC2 performed another 2 minutes of CC without audiovisual feedback at 30 minutes (CC3) and 5–7 days (CC4) later.
Results: The baseline compressions in target during CC1 was 14.43 ± 20.18%, improving significantly to 81.80 ± 7.61% (p < 0.001) with audiovisual feedback (CC2). Forty-five (90%) participants achieved compressions in target of at least 70% during CC2. However, without the feedback, compressions in target decreased significantly to 56.33 ± 27.02% (p < 0.001) and 49.32 ± 33.86% (p < 0.001) at 30 minutes (CC3) and 5–7 days (CC4) later, respectively. The overall effect size for the compressions in target was 0.625.
Conclusion: Audiovisual feedback device usage significantly improves CC performance, but improved skills were not fully retained when CC was performed without the device afterwards. Therefore, real-time audiovisual feedback may ensure better CC, a component of cardiopulmonary resuscitation.
References
Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary Resuscitation Quality: Improving Cardiac Resuscitation Outcomes Both Inside and Outside the Hospital: A Consensus Statement From the American Heart Association. Circulation. 2013;128(4):417–435. https://doi.org/10.1161/CIR.0b013e31829d8654
Panchal AR, Bartos JA, Cabañas JG, et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(16 suppl 2):S366–S468. https://doi.org/10.1161/CIR.0000000000000916
Abella BS, Sandbo N, Vassilatos P, et al. Chest Compression Rates During Cardiopulmonary Resuscitation Are Suboptimal: A Prospective Study During In-Hospital Cardiac Arrest. Circulation. 2005;111(4):428–434. https://doi.org/10.1161/01.CIR.0000153811.84257.59
Perman SM, Stanton E, Soar J et al. Location of In-Hospital Cardiac Arrest in the United States—Variability in Event Rate and Outcomes. J Am Heart Assoc. 2016;5(10). https://doi.org/10.1161/JAHA.116.003638
Resuscitation Training in Ministry of Health Malaysia. The Ministry of Health Malaysia. 2016. p. 36-38.
Bobrow BJ, Vadeboncoeur TF, Stolz U, et al. The Influence of Scenario-Based Training and Real-Time Audiovisual Feedback on Out-of-Hospital Cardiopulmonary Resuscitation Quality and Survival From Out-of-Hospital Cardiac Arrest. Ann Emerg Med. 2013;62(1):47-56.e1. https://doi.org/10.1016/j.annemergmed.2012.12.020
Aguilar S, Asakawa N, Saffer C, Williams C, Chuh S, Duan L. Addition of Audiovisual Feedback During Standard Compressions Is Associated with Improved Ability. West J Emerg Med. 2018;19(2):437–444. https://doi.org/10.5811/westjem.2017.11.34327
Cheng A, Magid DJ, Auerbach M, et al. Part 6: Resuscitation Education Science: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(16 suppl 2):S551–S579. https://doi.org/10.1161/CIR.0000000000000903
Snedecor GW, Cochran WG. Statistical Methods. 8th Edition. Ames: Iowa State Press; 1989.
Wutzler A, Bannehr M, von Ulmenstein S, et al. Performance of chest compressions with the use of a new audio–visual feedback device: A randomized manikin study in health care professionals. Resuscitation. 2015;87:81–85. https://doi.org/10.1016/j.resuscitation.2014.10.004
Pritchard J, Roberge J, Bacani J, Welsford M, Mondoux S. Implementation of Chest Compression Feedback Technology to Improve the Quality of Cardiopulmonary Resuscitation in the Emergency Department: A Quality Initiative Test-of-change Study. Cureus. 2019;11(8):e5523. https://doi.org/10.7759%2Fcureus.5523
Chelladurai G, Noor Azhar AM, Mohd Isa R, Bustam A, Ahmad R, Munisamy M. Improving cardiopulmonary resuscitation (CPR) performance using an audio-visual feedback device for healthcare providers in an emergency department setting in Malaysia: a quasi-experimental study. The Medical Journal of Malaysia 2020;75(5):514–518.
Lee JH, Cho Y, Kang KH, Cho GC, Song KJ, Lee CH. The Effect of the Duration of Basic Life Support Training on the Learners’ Cardiopulmonary and Automated External Defibrillator Skills. BioMed Res Int. 2016:2420568. https://doi.org/10.1155/2016/2420568
Abdullah Mahdy Z, Maaya M, Atan IK, Abd Samat AH, Isa MH, Mohd Saiboon I. Simulation in Healthcare in the Realm of Education 4.0. Sains Malaysiana. 2020;49(08):1987–1993. http://doi.org/10.17576/jsm-2020-4908-21
Hellevuo H, Sainio M, Nevalainen R, et al. Deeper chest compression – More complications for cardiac arrest patients? Resuscitation. 2013;84(6):760–765. https://doi.org/10.1016/j.resuscitation.2013.02.015
Beom JH, You JS, Kim MJ, et al. Investigation of complications secondary to chest compressions before and after the 2010 cardiopulmonary resuscitation guideline changes by using multi-detector computed tomography: a retrospective study. Scand J Trauma, Resus Emerg Med. 2017;25(1):8. https://doi.org/10.1186/s13049-017-0352-6
Cason CL, Trowbridge C, Baxley SM, Ricard MD. A counterbalanced cross-over study of the effects of visual, auditory and no feedback on performance measures in a simulated cardiopulmonary resuscitation. BMC Nursing. 2011;10(1):15. http://www.biomedcentral.com/1472-6955/10/15
Zhou X-L, Wang J, Jin X-Q, Zhao Y, Liu R-L, Jiang C. Quality retention of chest compression after repetitive practices with or without feedback devices: A randomized manikin study. Am J Emerg Med. 2020;38(1):73–78. https://doi.org/10.1016/j.ajem.2019.04.025
Merchant RM, Topjian AA, Panchal AR, et al. Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(16 suppl 2):S337-S357. https://doi.org/10.1161/CIR.0000000000000918