Keywords
Abstract
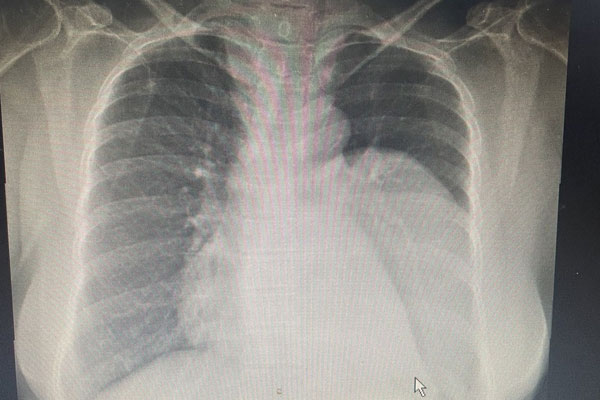
Neurofibromatosis type 2 (NF2) is a rare autosomal dominant disorder. We report a case of a 52-year-old woman with underlying NF2 who was scheduled for excision of cervical neurofibromas. The patient had four nerve sheath tumours affecting different parts of the airway, namely, two cervical neurofibromas with spinal cord compression, a large retrosternal goitre extending into the anterior mediastinal compartment causing central airway obstruction, and a large left thoracic paravertebral tumour in the posterior mediastinal compartment. After risk stratification and multidisciplinary discussion, awake nasal fibreoptic intubation with a contingency plan of rigid bronchoscopy and jet ventilation was decided. The patient was intubated successfully with target-controlled infusion remifentanil as the sole sedative and airway topicalization with local anaesthetic. The patient was ventilated in a prone position intraoperatively with no desaturation. The tumours were successfully removed and the patient was discharged well. Awake nasal fibreoptic intubation is the choice of management in difficult airways affected by multicompartmental tumours in a centre that is devoid of extracorporeal membrane oxygenation service.
References
Tamura R. Current understanding of neurofibromatosis type 1, 2, and schwannomatosis. Int J Mol Sci. 2021;22(11):5850. https://doi.org/10.3390/ijms22115850
Guedes F, Branquinho MV, Sousa AC, Alvites RD, Bugalho A, Maurício AC. Central airway obstruction: is it time to move forward? BMC Pulm Med. 2022;22(1):68. https://doi.org/10.1186/s12890-022-01862-x
Anderson DM, Dimitrova GT, Awad H. Patient with posterior mediastinal mass requiring urgent cardiopulmonary bypass. Anesthesiology. 2011;114(6):1488-93. doi: https://doi.org/10.1097/ALN.0b013e31821a8af1
Datt V, Tempe DK. Airway management in patients with mediastinal masses. Indian J Anaesth. 2005;49(4):344-52.
Lin J, Frye L. The intersection of bronchoscopy and extracorporeal membrane oxygenation. J Thorac Dis. 2021;13(8):5176-82. https://doi.org/10.21037/jtd-2019-ipicu-08
Erdös G, Tzanova I. Perioperative anaesthetic management of mediastinal mass in adults. Eur J Anaesthesiol. 2009;26(8):627-32. https://doi.org/10.1097/EJA.0b013e328324b7f8
Hensley Jr, DE, Martin DE, Gravlee GP, editors. A Practical Approach to Cardiac Anesthesia, 5th ed, FA. Philadelphia, PA: Lippincott, Williams and Wilkins, 2013.
Johnston KD, Rai MR. Conscious sedation for awake fibreoptic intubation: a review of the literature. Can J Anaesth. 2013;60(6):584-99. https://doi.org/10.1007/s12630-013-9915-9